MIS Posterior Percutaneous Instrumentation
This procedure is usually performed to add stability for any lumbar interbody fusion (Anterior lumbar fusion, Lateral lumbar fusion, Transforaminal lumbar fusion, Oblique lumbar fusion, Endoscopic lumbar fusion). Dr. T uses the minimally invasive technique, and the surgery is done through a 1-inch incision on each side of the midline of your lower back. This approach allows Dr. T to place screws using the natural muscle plane rather than detaching or removing muscle from the underlying bone.
These are the steps:
- Fluoroscopic X-rays are used to localize the pedicle insertion point, and a Jam-Shidi needle is placed through the pedicle and into the vertebral body under image guidance.
- The inside of the Jam-Shidi needle is removed, and a longer guide wire is placed through the outer cannula of the Jam-Shidi needle into the anterior part of the vertebral body.
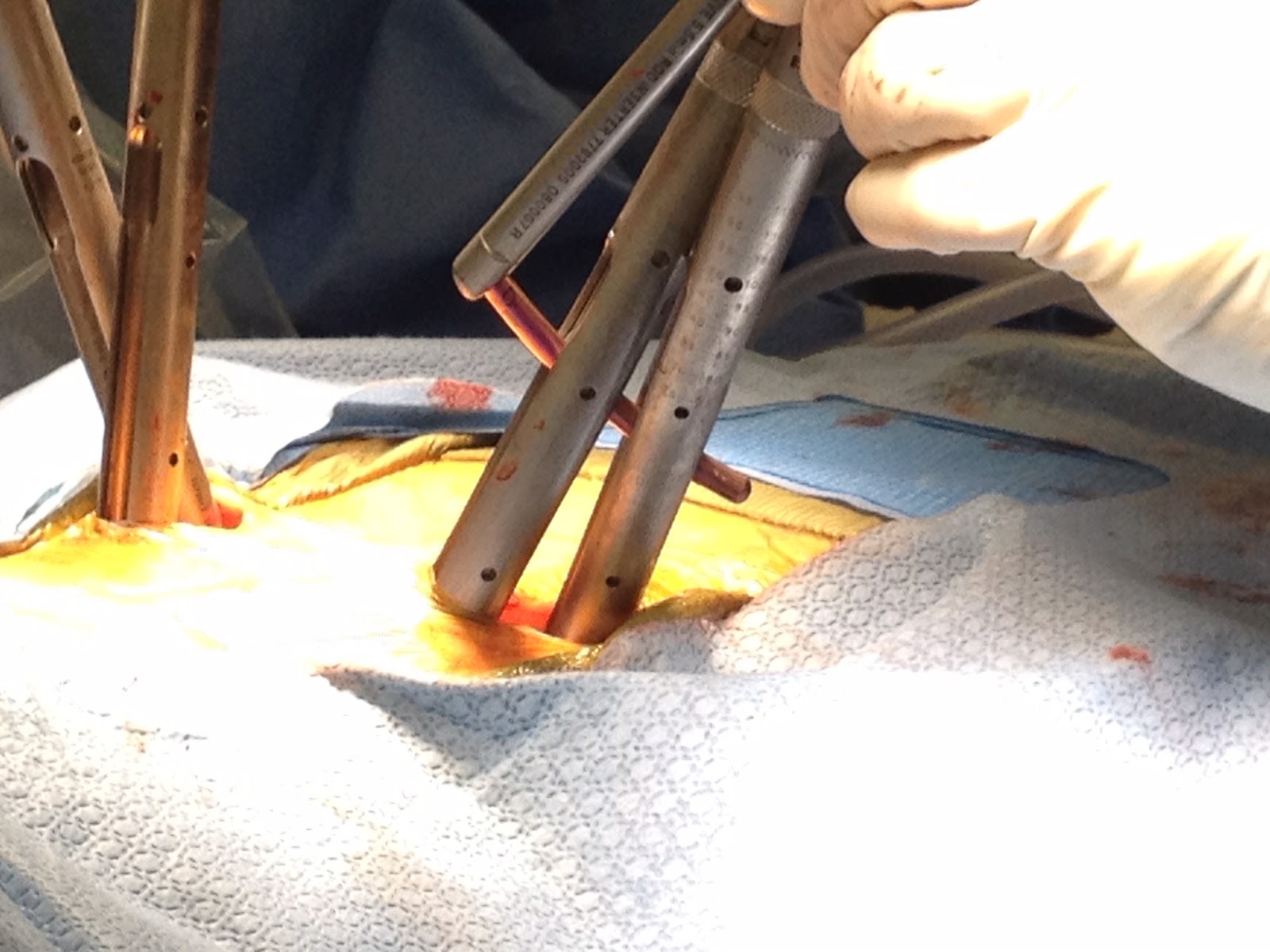
- Soft tissue dilators are placed sequentially with increasing diameters to secure the soft tissue minimally invasive corridor. The wire can now be tested electro-physiologically to ensure there is no contact with a spinal nerve.
- A cannulated tap is deployed over the guide wire to prepare the path for the pedicle screw. The tap is tested continuously in real-time to ensure the pedicle wall is not breached and there is no proximity to a spinal nerve.
- Minimally invasive titanium screws are inserted with attached sleeves. The sleeves are used to guide the rod to the screw heads. This process is repeated for as many screws as are needed.
- Finally, the rod is delivered through the screw sleeves, locking caps are screwed into the screw heads on top of the rod, locking the rod to each screw. The sleeves are disconnected from the screw heads to leave behind the final construct of pedicle screws and rods.
- The incisions are re-approximated with sutures, and the skin is closed using “skin glue”.
Benefits associated with a MIS Posterior Percutaneous Instrumentation:
- Minimally invasive technique – less trauma to muscles and soft tissue than with traditional open surgery
- Fast recovery time
- Minimal pain or discomfort following the surgery
- Fewer complications than open spine surgery
- Small incision and minimal scar tissue
- High success rate and sustained success of the therapy
- Minimal blood loss
What to expect after the procedure?
While this is an outpatient surgery, we do recommend resting for a prescribed period post-operative and then gradually increasing activity levels with instruction and supervision by your providers. You will also be advised to wear a back brace for added support during the healing process.
