Endoscopic Decompression
An endoscopic micro-invasive decompression is the least invasive technique that allows direct visualization of the disc and the nerves. This procedure is used for decompressing nerve roots damaged by narrowing of the spinal canal and foramina caused by bulging discs, herniated discs, facet arthritis, bone spurs, scoliosis, and spondylolisthesis.
It is typically indicated in patients with neurological symptoms such as radiating leg pain, tingling, numbness, weakness, difficulty breathing, and in some cases, bowel or bladder problems. Most of our patients have not found adequate relief with non-surgical modalities, including pain management injections or other conservative treatments. This procedure can also help relieve pain associated with spinal stenosis and low back arthritis.
What is an Endoscopic Decompression?
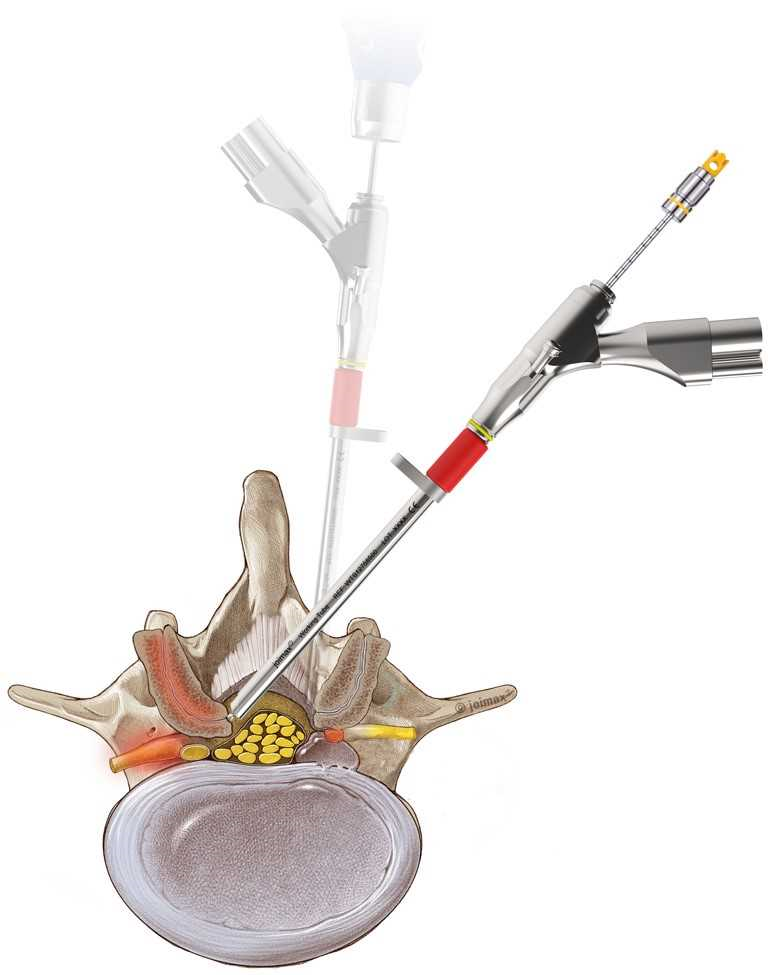
An endoscopic decompression is the least invasive surgery that allows the surgeon to decompress spinal nerves in the spinal canal using an incision smaller than 1 cm. The surgery uses an endoscope, real-time EMG, and real-time radiographic images, making it very safe and effective.
Many patients who suffer from sciatica, referred leg pain, or low back pain may be candidates for this procedure. It can also relieve pain associated with spinal stenosis and low back arthritis.
Benefits of Micro-Invasive Endoscopic Decompression
- Least invasive technique – minimal trauma to muscles and soft tissue
- Fast recovery time
- Minimal pain or discomfort after surgery
- Immediate leg pain relief in most cases
- Fewer complications and risks than traditional open spine surgery
- Small incision and minimal scar tissue
- High success rate and long-term relief
- No or minimal blood loss
- No hardware placement or loss of mobility
Indications for Endoscopic Micro-Invasive Decompression
- Spinal canal narrowing due to stenosis
- Bulging or herniated discs, facet arthritis, bone spurs, scoliosis, and spondylolisthesis
- Severe back or leg pain with neurological symptoms
- Failure of conservative treatments
Details of the Procedure
Micro-invasive endoscopic decompression requires a small incision (usually no larger than 1 cm) and x-ray guidance to access the lumbar spine.
Under x-ray guidance, a series of muscle dilators are used to gently separate soft tissue rather than cutting through muscle. This creates a path for the endoscope. Specialized tools may also be used to remove arthritic bone compressing the spinal nerves. The goal is to free up the nerves in the spinal canal. This surgery is performed under general anesthesia and typically lasts 2–3 hours, depending on the complexity.
