You may be a candidate for Lumbar Disc Replacement
Lumbar Degenerative Disc Disease
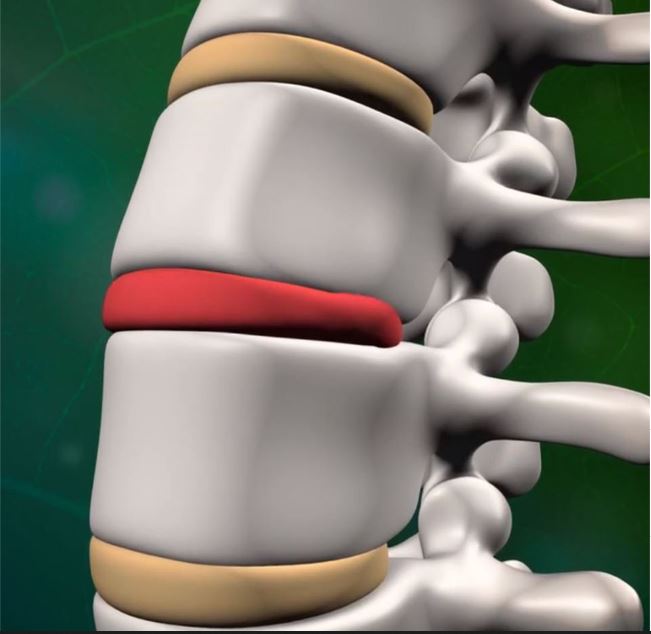
The spine, also known as the “backbone,” protects the spinal cord, bears the weight of the body, and facilitates movement. Vertebral bones, stacked atop one another, form the spinal column. Most of the vertebrae are separated by intervertebral discs, which are made up of cartilage and fibers. These discs account for almost ¼ of the spine’s length, absorb shock and strain, and cushion the spine as it flexes, twists, and bends.
Although intervertebral discs are almost entirely comprised of water, collagen, and proteoglycans, these three components are present at different levels between the disc’s exterior and interior. Because the nucleus of the disc contains a substantial amount of water, it is soft, gel-like, and liquefied. This gelatinous center is surrounded by a hard, protective outer casing.
Despite having this supportive outside, intervertebral discs are still very vulnerable to damage. As we age, our spines begin to lose water content and then deteriorate. Discs begin to compress, tear, or rupture. “Degenerative disc disease” refers to this natural process, wherein general wear and tear negatively affect the intervertebral discs as a person grows older.
Degenerative disc disease most often occurs in the lower back (known as the lumbar spine) and neck (known as the cervical spine) and can cause pain, pressure, and nerve damage. If left untreated, degenerative disc disease can cause serious and debilitating spinal issues. Spinal stenosis, herniated discs, collapsed discs, spinal cord injuries, and other severe complications sometimes originate from degenerative disc disease.
Degenerative Disc Causes
There is one prominent cause of degenerative disc disease, and that is the natural effects of aging on the intervertebral discs in the spine. However, certain medical factors can exacerbate and intensify degenerative disc disease, including:
- Smoking
- Lack of exercise
- Obesity or carrying excess weight
- Improperly lifting heavy objects
- Making repetitive, strenuous movements
- A sudden, serious injury, such as one that may result from a fall, car accident, or high-impact sport
Osteoporosis, herniated discs, spinal stenosis, and other spinal complications can surface as a result of degenerative disc disease. If you believe you may be at risk for degenerative disc disease, speak with your doctor about how to maintain long-term spinal health. By practicing proper precautions and making certain lifestyle changes, you can reduce your risk of contracting premature spine-related difficulties while proactively warding off issues later in life.
Degenerative Disc Symptoms
As with most back, neck, and spine issues, degenerative disc disease is associated with a variety of symptoms and can easily be confused with another condition. If you suspect you may be suffering from degenerative disc disease, schedule a consultation with one of our Board-certified spine surgeons to attain a comprehensive, accurate diagnosis. Some of the symptoms attributed to degenerative disc disease include:
- Acute or chronic neck or back pain that may be dull and aching or sharp and pronounced
- Limited mobility and discomfort when trying to participate in everyday activities
- Neck or arm pain, if the damaged disc is located in the neck
- Back, buttock, and leg pain, if the damaged disc is located in the lower back
- Pain that worsens when bending, reaching, sitting, or twisting
Our Microspine & Minimally Invasive Treatment Approach
Although degenerative disc disease affects many men and women as they grow older, you do not have to accept debilitating symptoms as a permanent aspect of your daily life. Dr. T is committed to helping you find safe and compassionate solutions for your degenerative disc disease symptoms. By providing personalized, state-of-the-art care, we strive to ensure that patients return to their everyday lives without being hindered by pain or the fear of developing secondary complications.
During your initial consultation, Dr. T will carefully evaluate your medical history and physical state. To obtain a comprehensive and clear diagnosis, imaging tests like a CT scan, X-ray, or MRI may be requested. Based upon the information gathered, we will design a personalized treatment plan tailored to meet your unique needs.
Whenever possible, we usually recommend undergoing a combination of conservative treatments before exploring surgical options. Frequently, patients experience significant relief from degenerative disc disease-related symptoms through:
Physical Therapy and Exercise: It may seem counterintuitive, but bed rest does not typically help men and women suffering from degenerative disc disease and other spine complications feel better. By strengthening the abdominal muscles, losing excess pounds, and improving your flexibility, you can reduce some of the strain placed upon your spine. Moderate, targeted exercise may provide dramatic relief from the effects of degenerative disc disease and can help prevent the development of secondary conditions.
Medication: Over-the-counter or prescription medication may be recommended to reduce the inflammation associated with degenerative disc disease. Cortisone injections may also be implemented, which provide pain-relieving agents directly to the affected region. Although medication is not a life-long solution for degenerative disc disease, physician-directed medicinal use can give patients the respite they need to implement exercise and other long-term treatments.
Additional Methods: The use of ice packs, heating pads, and other non-invasive treatments can sometimes eliminate or alleviate degenerative disc disease symptoms.
Some patients might need spinal injections such as epidural injections.
If conservative treatments do not provide adequate relief, Microspine endoscopic disc repair may be necessary. Some patients might need stabilization or fusion surgery whereas other patients might be candidates for artificial disc replacement.
When compared with traditional open operations, our Microspine & Minimally Invasive technique yields:
- Shortened recovery times that allow patients to return to work, school, and other daily activities faster
- Less post-operative pain
- A reduced risk of scarring and blood loss
- Minor trauma to surrounding tissues, leaving the majority of muscle unaffected
- Fewer potential complications
We look forward to helping you feel better, faster! CONTACT US
