You may be a candidate for Endoscopic Discectomy
Herniated Disc
If you’re suffering from a herniated disc, you’re not alone. Many men and women experience a herniation at some point in their lifetime, often without realizing it until the appearance of persistent and palpable symptoms. Becoming well informed about your condition is the first step toward finding a potential treatment and resuming a pain-free life. We’re here to help!
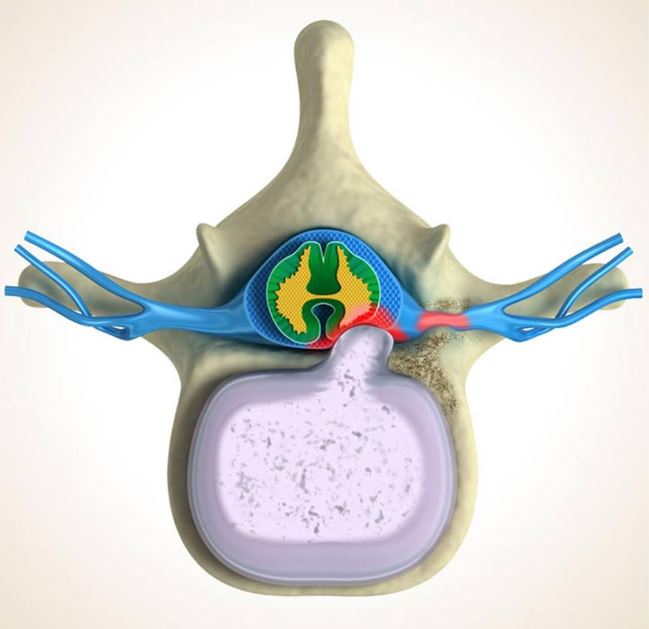
So, what precisely are the “discs” causing you so much trouble? Discs are shock absorbers located between vertebrae that cushion the spinal column and protect the spine from everyday strain. Made from a hard outer layer known as the annulus and a soft, liquid-like material known as the nucleus, discs usually do us a whole lot of good. Occasionally, however, a tear or weakness in a disc’s outer layer allows the fluidic inner layer to leak into the spinal canal. As a result, additional pressure is placed on local nerves, causing pain, discomfort and other complications. This ailment is known as a herniation, or a slipped or ruptured disc.
Herniated Disc Symptoms
Symptoms of a herniated disc vary widely and are determined by where the problem area is located within the spine. Sometimes, patients may exhibit no outward signs of a ruptured disc at all. When the disc begins to strain a nearby nerve, however, typical symptoms called “Sciatica” but additional symptoms include:
- Dull, achy pain or sharp, intense pain
- Muscle tightness and cramping
- Radiating pain through the down the legs
- Tingling sensations through the legs or down the foot
- Weakness in the affected area and limbs
- Lower back pain that gets worse when you sit, cough or sneeze
Herniated Disc Causes
If you have any of the above indicators, you may be bearing a herniated disc. Sometimes, patients can remember the precise moment when the damage most likely occurred; others are at a loss to understand how they could have contracted such a problem. The most common causes of a slipped disc are the following:
- Degenerative disc disease
This complication occurs when the discs in the spine lose volume over time and do not properly absorb shocks or allow the spine to flex and twist. Weak discs are more likely to rupture.
- Sudden trauma or accident
Occasionally, an abrupt and unexpected injury can cause a slipped disc when the body is forced to contort or external forces place unbearable pressure upon the spine.
- Frequent, improper movements or lifting
When you lift things incorrectly by bending (instead of squatting) or try to carry heavy loads beyond your capacity, you may herniated a disc.
Certain factors can increase your likelihood of getting a herniation, such as overweight, which places extra stress on the discs in your lower back. Some people also inherit a genetic predisposition to slipped discs or have an occupation where repetitive, strenuous motions raise their chances of harm. Additionally, if you are a smoker, you are also at risk for herniated discs.
Herniated Disc Non-Surgical Treatment Options
There are many methods available to treat disc ruptures. Depending on the location and severity of your injury, you may consider:
- Therapy
Often, licensed physical therapists can teach you positions and exercises to alleviate herniated disc pain. By strengthening the back and abdominal muscles, you may relieve some of the strain on the ruptured disc and minimize inflammation. Traction, electrical stimulation and short-term bracing may also improve your condition. “Hot and cold” therapy, where heating and cooling elements are applied to the affected area, is often utilized by many professionals as well. You can carry out this method by taking hot showers or baths and using ice packs or heating pads.
- Medication
Some prescription and over-the-counter medications may temporarily minimize the discomfort caused by herniated discs. Before you implement either, however, speak with your doctor. Certain medications can make your condition worse and may lead to other serious consequences.
- Lifestyle changes
By mindfully approaching your everyday life, you can prevent herniated discs and encourage those you already have toward healing. Bed rest is not recommended. Do not participate in intense exercise, particularly heavy lifting, if there is acute back pain. Get plenty of sleep. Many men and women are able to reduce the pressure on their back through intentional yoga practice.
Lumbar Herniated Disc Microspine & Minimally Invasive Treatment Options
If the above treatments do not provide permanent respite from the symptoms of your herniated disc, Microspine Endoscopic discectomy may be required. Dr. T will work with you to create a customized treatment plan based on your individual preferences and needs. Microspine & Minimally invasive procedures require only a small incision and generally lead to a much shorter recovery time than traditional open surgery, because they place less trauma upon muscles and tissues surrounding the affected area.
Our highly trained physicians use advanced techniques to treat slipped discs and degenerative disc disease. Here are just a few of the minimally invasive procedures we perform:
Endoscopic Lumbar MicroDiscectomy
This is the most advanced technique that can be done outpatient under general anesthesia and sometimes under sedation (twilight). The surgery is performed through a 1-cm incision (about size of a pen). Dr. T utilized high definition/high magnification scope and special tools to shrink, and trim the pathological disc in order to relieve pressure on surrounding nerve roots. The disc wall is then sealed to prevent further leakage and continuing pain. The stable portion that still function as a cushion in the center will be left intact; thus no fusion, screws/rods, and hardware needed.
Endoscopic OR MIS-Lumbar Stabilization/Fusion
This is the most advanced technique that can be done outpatient under general anesthesia in healthy patients. The indications are failed prior surgeries, severe collapsed disc, and unstable spine.
When compared with traditional open operations, our Microspine & Minimally Invasive technique yield:
- Shortened recovery times that allow patients to return to work, school and other daily activities faster
- Less post-operative pain
- A reduced risk of scarring and blood loss
- Minor trauma to surrounding tissues, leaving the majority of muscle unaffected
- Fewer potential complications
We look forward to helping you feel better, faster!
